It was November 2019 and the Fangman family had just finished Thanksgiving dinner with their six children. Their youngest, Katie, was an active toddler and had been pretty healthy for her first 20 months of life. That day, Nicole, a former critical care nurse, and Ben, a physician, noticed Katie was a little tired, had a runny nose and a small cough, but didn’t think too much of it.
“Being a doctor and a nurse, we are a tiny bit overprotective,” Nicole laughs. “I had Ben listen to Katie’s lungs before putting her down to bed that night and he didn’t notice anything unusual.”
The next morning as Ben walked into Katie’s room to get her up for the day, he didn’t realize his whole life was about to change.
Ben looked down into the crib and Katie was lethargic and unresponsive.
“We didn’t know what was going on,” explains Nicole. “I thought in my head, did she eat something, did she get poisoned somehow? We just had no idea what was going on. It was a nightmare, and we were so scared.”
Nicole and Ben immediately scooped her up and knew they needed to head to the Emergency Department at Children’s Nebraska, which was thankfully less than a 15-minute drive away.
Upon arriving to the hospital, Katie’s oxygen levels were dangerously low. Children’s team took a chest X-ray which showed she had a bad pneumonia and acute respiratory distress syndrome. Katie was immediately given oxygen.
“Everything happened so fast. They put her on the strongest oxygen possible through a mask,” remembers Nicole. “Then, before you knew it, we were in the Pediatric Intensive Care Unit (PICU). We just didn’t know what on earth was going on.”
Katie’s case baffled the doctors, too, since she was previously healthy. They began running tests to try to understand what was going on, and eventually had to intubate Katie due to her needing more and more oxygen.
Soon after, bloodwork came back and revealed Katie had respiratory syncytial virus (RSV) and pneumonia, which had been setting in for several weeks. The doctors concurred that the combination of these two diagnoses must have taken out her immune system overnight, causing her to become so sick.
“We were so scared and were worried they wouldn’t be able to find a way to treat her,” says Nicole. “The doctors were quickly trying to figure out the next steps and put a plan together for Katie because she was going downhill quickly.”
Soon, the topic of extracorporeal membrane oxygenation (ECMO)—the most advanced form of life support—was brought up. ECMO is commonly used for heart patients, but the team discussed putting Katie on a special kind of ECMO called Veno-Venous (VV) ECMO, specifically for respiratory patients. For Katie, ECMO would be used to bypass her lungs and oxygenate her blood outside of her body so her lungs could recover. Because Katie was at Children’s, a team was immediately able to be assembled to begin treatment.
“All I remember was as soon as ECMO was mentioned, there was a huge team of people at the bedside within about five minutes. It was amazing to me how quickly the team was able to come together,” remembers Nicole.
Children’s Nebraska is the only children’s hospital in the region to offer ECMO for infants, children and teens, and specialize in this treatment for critically ill pediatric patients. Katie had come to the right place. Children’s PICU is designated as a Center of Excellence in life support, with processes, procedures and systems in place that promote excellence and exceptional care in providing ECMO to young patients. The team also collaborates with professional organizations like Extracorporeal Life Support Organization (ELSO), an international group of professionals who share data and information about ECMO use.
Katie remained on ECMO for 53 days, the longest any patient has stayed on ECMO at Children’s.
“The treatment was touch and go for a while. I remember just holding Katie’s hand and praying that it would work,” says Nicole. “Katie was on heavy sedatives and would get chest X-rays every day. It wasn’t until right after the new year that we would have a huge break in Katie’s treatment.”
Katie would regularly receive chest X-rays, but in January 2020, she received a CT scan that revealed large abscesses from her pneumonia in her lungs. She was put on antibiotics and the nurses would suction her every day. One day, a nurse was suctioning her, and miraculously, a large clot came out.
“That was our turning point!” explains Nicole. “It was amazing. Her airways opened and her lungs started moving air. At that point, things were a lot better, and we were able to take her off ECMO. I finally got to hold her for the first time after two months and held her for eight straight hours.”
Although there were still a few setbacks, Katie was eventually able to move down to the step-down unit and start weaning off the medications and begin rehab. Her brothers and sisters even got to come visit her in February to celebrate her second birthday.
“It was amazing to watch her brothers and sisters interact with her. She had this balloon, and she would hit each of them on the head with it when we said their name,” Nicole explains. “It was during this exercise that we knew Katie had full brain function because she was able to remember everyone’s names. I was so relieved!”
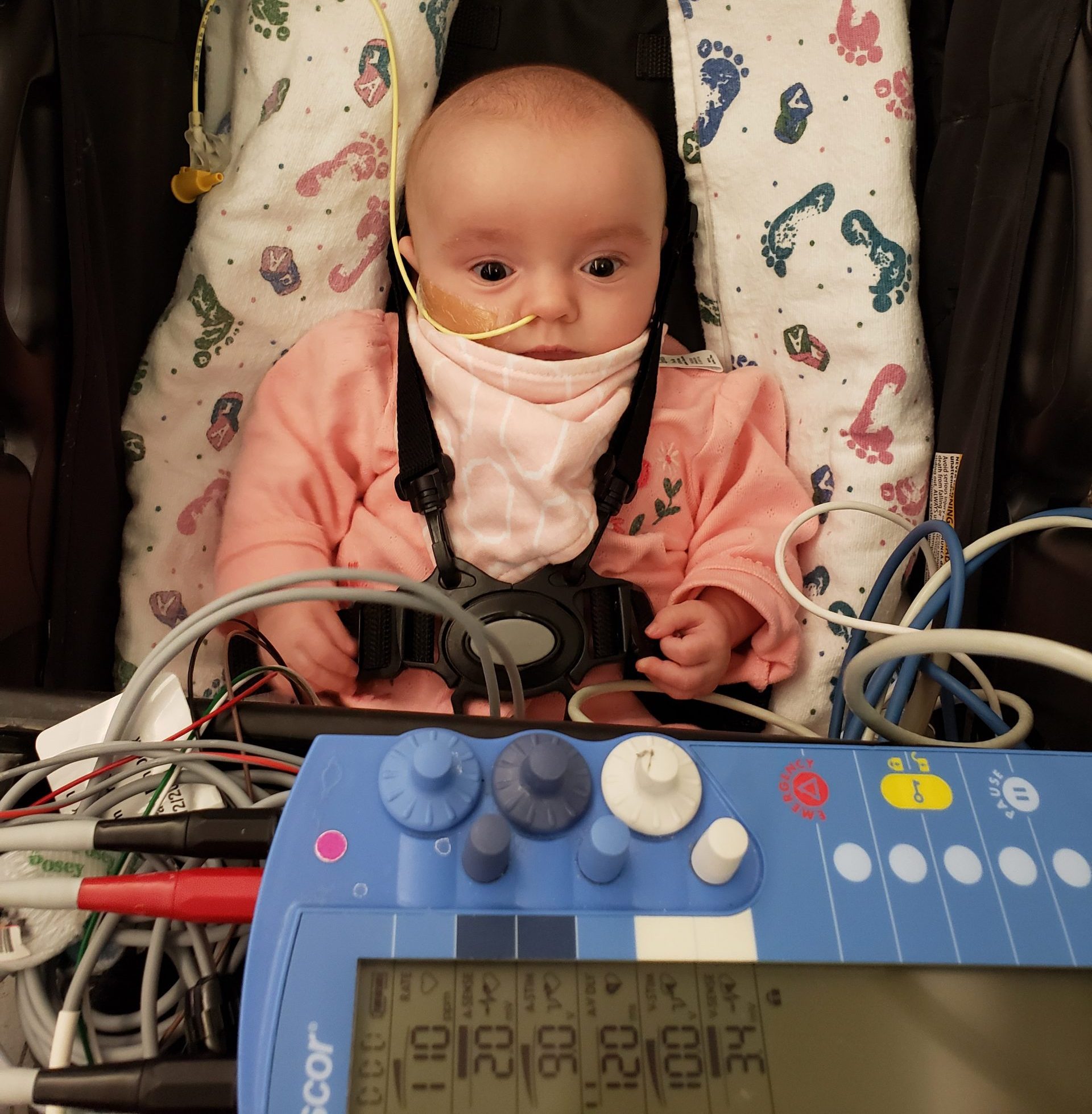
Katie did have to receive a tracheotomy after coming off ECMO which helped her to be able to move around even with the ventilator. She did so well at rehab that her nurses called her “the miracle child,” and within a couple of months and intense rehab, Katie was even able to get the trach out.
“The doctors told me there was something very special about her recovery,” says Nicole. “I Can’t begin to thank the doctors and nurses in the PICU enough for everything they did to get Katie home. They took care of her, and they took care of us. They just didn’t miss a beat, and it was amazing. They are special people and truly do it for the kids.”
Katie was treated in the current PICU at Children’s, but in late August 2021, a newly renovated 32-bed PICU will open in the Hubbard Center for Children. The same highly trained and specialized staff will be on the unit, but the space will feature rooms with more natural light and larger sleeping areas for parents who are staying overnight.
Children’s PICU offers a full range of pediatric medical and surgical specialists, in departments from neurology to cardiology, and is continuously staffed by physicians, nurses and other providers who are trained in the care of children with critical illness and injury. Compared to other PICUs of similar size across the country, the patient outcomes are among the best. Children’s also has a Critical Care Transport Team with specially trained emergency medical technicians and registered nurses who transport critically ill patients up around the region and across the country. With the addition of the PICU in the Hubbard Center, Children’s will have one of the largest PICU bed counts in the region.
“I am so impressed with what I see happening at The Hubbard Center. It is going to be so nice to have a building dedicated to the PICU,” says Nicole. “It is going to be a game changer to have everything together and have all the facilities right there like the operating rooms, testing areas and radiology. I love the design and love how modern and fresh everything looks.”
Today, Katie is a thriving 3-year-old and not having any issues after being in the hospital for all those months.
“She is such a girly girl. She loves Barbies and Peppa Pig and dressing up,” said Nicole. “She loves running after her white fluffy dog and doing all kinds of crafts and painting. I am so glad we have our little girl back. If it wasn’t for our wonderful nurses, Hannah, Rachael and Ashley, and the amazing doctors like Dr. Ortmann, Dr. Solomon and Dr. Norton, I honestly don’t know if she would be here today. I just feel so blessed to be in a state that has a hospital like Children’s that has the capabilities to take care of complex patients like Katie, and I look forward to seeing what the Hubbard Center will bring to our city.”




 When Mathís was a little over a year old, the McCullens, who are from Omaha, noticed a ridge on their son’s forehead. It did not seem to bother Mathís, and the McCullens weren’t too concerned. They thought it was a minor imperfection their son was born with, until a family in one of their online parenting groups reached out to them.
When Mathís was a little over a year old, the McCullens, who are from Omaha, noticed a ridge on their son’s forehead. It did not seem to bother Mathís, and the McCullens weren’t too concerned. They thought it was a minor imperfection their son was born with, until a family in one of their online parenting groups reached out to them. In August 2021, Kristin and Monét met with
In August 2021, Kristin and Monét met with  According to
According to  Just before his second birthday, Mathís had skull surgery on Nov. 3, 2021. The six-hour operation involved making an incision along his scalp, opening up and removing the top half of his skull and separating the skull from the dura and opening to his brain. After removing the affected bone,
Just before his second birthday, Mathís had skull surgery on Nov. 3, 2021. The six-hour operation involved making an incision along his scalp, opening up and removing the top half of his skull and separating the skull from the dura and opening to his brain. After removing the affected bone,  “
“


 To promote healing, Jesse had to wear arm splints to keep him from putting his fingers and sharp, pointy objects in his mouth, which could damage the sensitive tissues in his palate. Now that his palate has healed completely, Jesse is a happy baby who loves to eat and talk.
To promote healing, Jesse had to wear arm splints to keep him from putting his fingers and sharp, pointy objects in his mouth, which could damage the sensitive tissues in his palate. Now that his palate has healed completely, Jesse is a happy baby who loves to eat and talk.