Game-changing collaboration gives 6-year-old Beaudin freedom from epileptic seizures.
When a child’s epilepsy proves drug-resistant, families may feel unsure of where to turn next. For 6-year-old Beaudin’s parents, Nick and Catelyn, the solution for their son’s epilepsy was found through Children’s Nebraska’s expert Neurosciences team, which offers the most comprehensive pediatric epilepsy care for children and families across the region.
Beaudin had a rare form of epilepsy that affected him as he slept. Despite multiple different medications, two rounds of steroids and multiple electroencephalographies (EEG), Beaudin’s days were still marked by a heightened need to sleep. A seizure at school, more testing and his fourth failed medication prompted his pediatric neurologist at Children’s, Rhonda Wright, M.D., to refer the concerned family to Sookyong Koh, M.D., Ph.D., an epileptologist and Children’s division chief of Pediatric Neurology, and Afshin Salehi, M.D., M.S., a pediatric neurosurgeon and Children’s surgical director of epilepsy. His parents also spoke with a contact at the Epilepsy Foundation of Nebraska, who affirmed Dr. Koh and Dr. Salehi’s expertise.
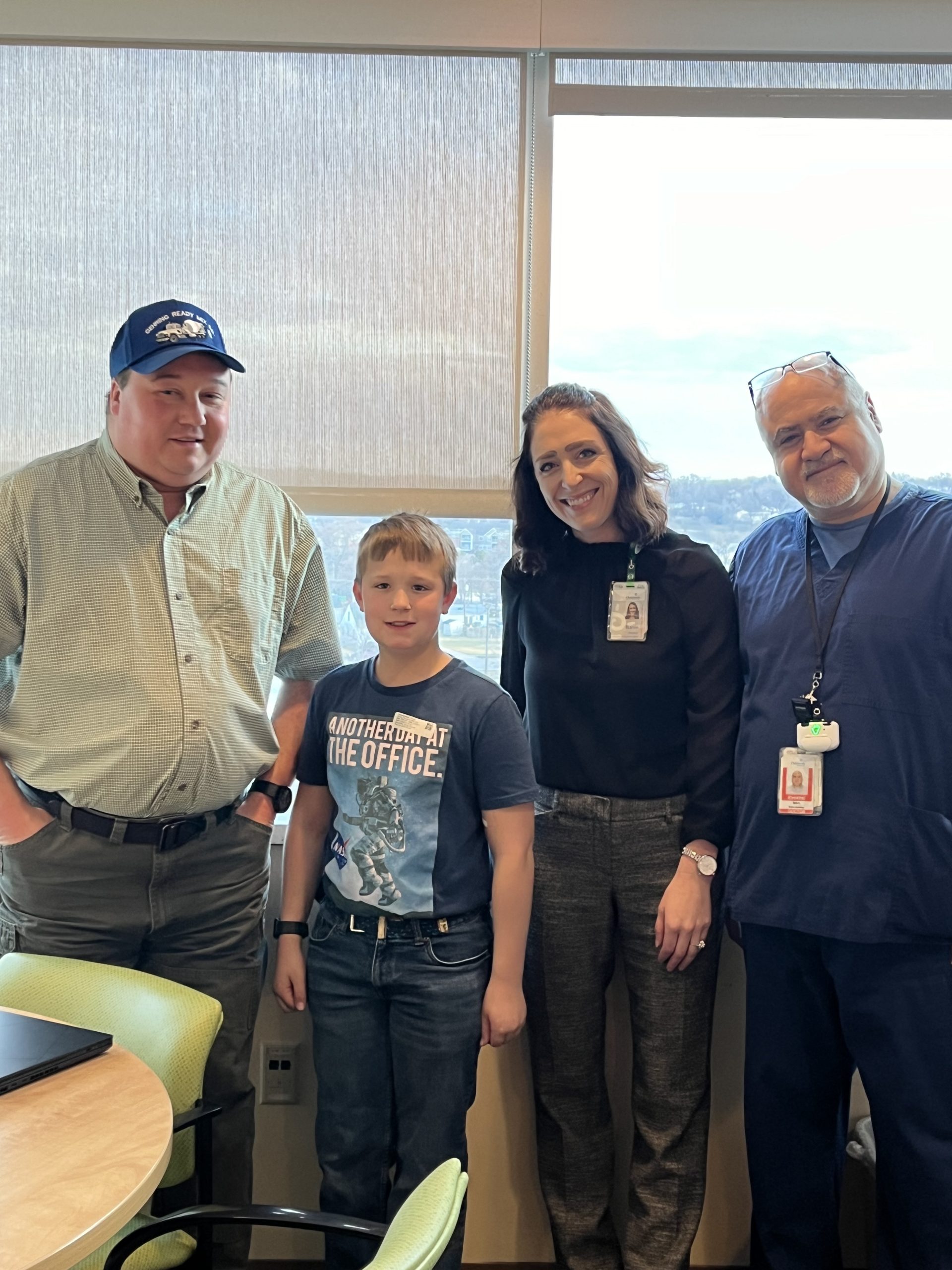
Just days later, Beaudin’s parents connected with Dr. Salehi, Dr. Koh and another epileptologist, Spriha Pavuluri, M.D., through the innovative Drug Resistant Epilepsy Clinic inside Children’s Neurosciences Center. The trio collaborated to find the right treatment option for Beaudin and his drug resistant epilepsy, which is characterized by epileptic seizures that don’t respond to at least three medications. Continued assessment through a series of scans ultimately confirmed surgery was the right course of action for Beaudin.
“It was so hard because Beaudin wasn’t his normal self, and he was falling asleep more,” says Catelyn. “I kept wondering how long we’d have to try all these medications and changes. It was a relief when Dr. Wright referred us to Dr. Koh and Dr. Salehi because I knew we were going to be taken care of. Nick and I knew surgery was the right choice to help Beaudin.”
In May 2023, Dr. Salehi placed recording electrodes in Beaudin’s brain with subdural grids and strips—a first at Children’s—which allowed the Neurodiagnostics team to observe Beaudin’s brain activity intracranially, or directly from the brain. Dr. Pavuluri led brain mapping for five days, with the team inducing seizure activity to gauge the origin and where it affected Beaudin’s motor sensory area, leading to more precise localization compared to a non-invasive (scalp) EEG.
Days later, Beaudin went back to the operating room, and Dr. Salehi removed the grids and strips. He then completed a craniotomy to resection Beaudin’s brain in the frontal and parietal lobes, disconnecting the nerves that were causing the seizures—all with active, real-time guidance from Children’s epileptologists. The surgery was an immediate success.
“We were able to provide expedited and effective care for Beaudin, and his life post-surgery has dramatically improved,” says Dr. Salehi. “Our close collaboration between the epileptologists and the pediatric epilepsyneurosurgeon is everything, and we’re proud to offer a level of pediatric epilepsy care that is not available anywhere else in the region.”
Beaudin left the hospital two days after surgery. Four days post-operation, Catelyn allowed him to take a baseball bat outside, curious to see the progress of his motor skills. Beaudin swung the bat with gusto, a sign he had regained strength and motor function.
Surgery—once a frightening prospect for his parents—had changed his life.
“We knew we could offer Beaudin and his family more,” Dr. Pavuluri says. “We’re not just going to stop at medications and sit on the sidelines. We’re able to offer more with newer modalities and innovations that were not even available until a couple of years ago, helping kids like Beaudin have better outcomes, experiences and an improved quality of life.”
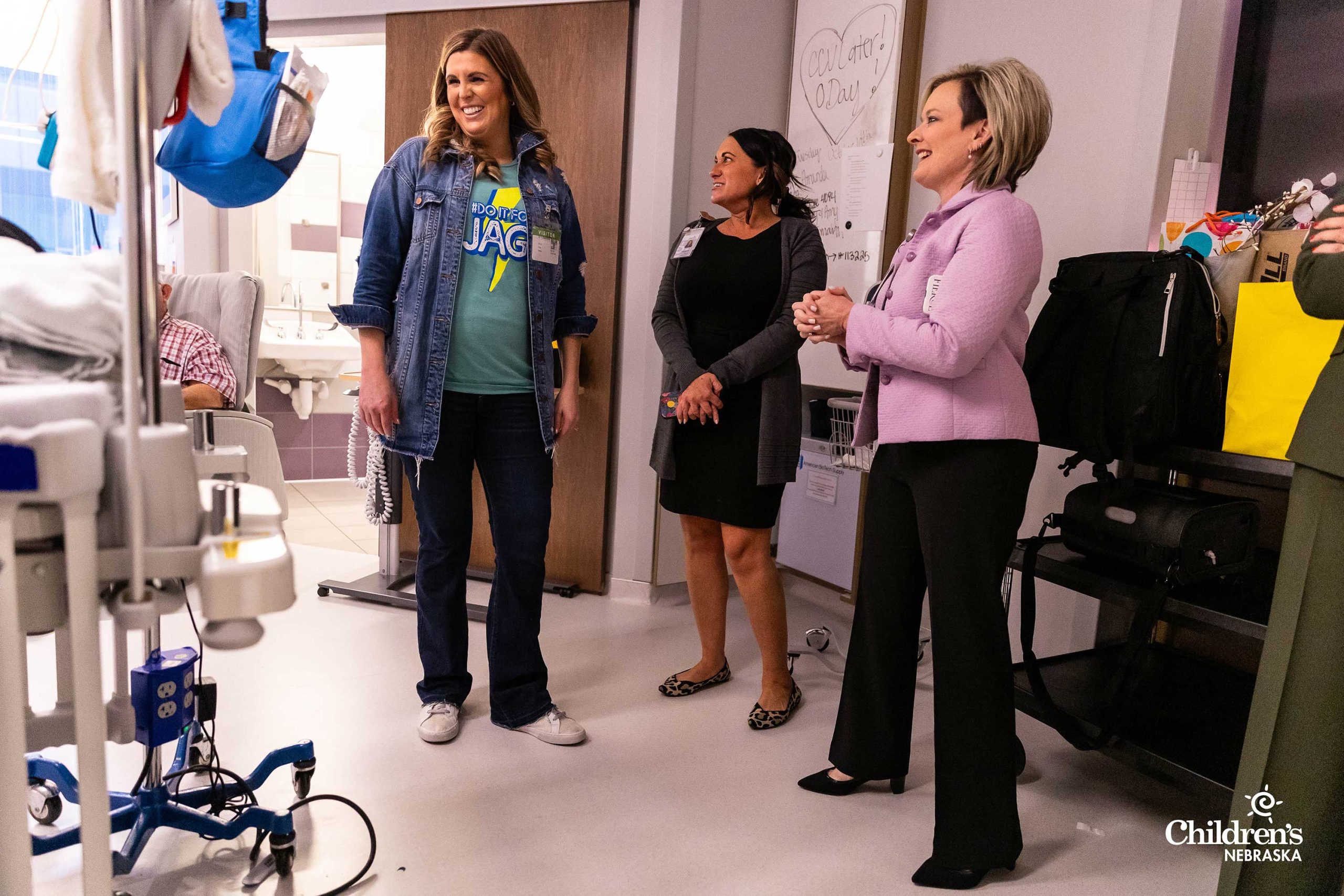
Now a year out from surgery, Beaudin is thriving. The energetic, personable rising first grader loves playing baseball and is joining his teammates on the diamond again this summer.
“People have told us you’d have no clue that Beaudin has had major brain surgery unless you saw the scar on his head,” Catelyn says. “Surgery is a huge, scary word sometimes, but it was our last resort. This was the best decision we’ve ever made for our son, and it’s absolutely something families should consider.
“We have faith and trust in our Children’s care team. The Drug Resistant Epilepsy Clinic team is so well versed and knowledgeable, and they truly go through every hoop to make sure surgery is the right option. They were very thorough in confirming that this was best for Beaudin. I Can’t thank Dr. Koh, Dr. Pavuluri, Dr. Salehi and their team enough. Beaudin will have a much better life because of this.”































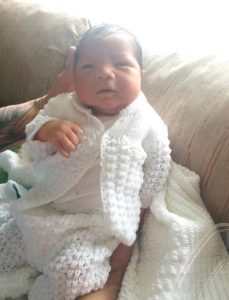 On April 14, 2021, Dulce gave birth to Bellamy in Grand Island, Neb. The Pantojas were so happy to see their baby boy as he let out a loud cry. But the constant pushing and excessive force during childbirth caused trauma to the baby, and as a result, Bellamy lacked total movement in his left arm.
On April 14, 2021, Dulce gave birth to Bellamy in Grand Island, Neb. The Pantojas were so happy to see their baby boy as he let out a loud cry. But the constant pushing and excessive force during childbirth caused trauma to the baby, and as a result, Bellamy lacked total movement in his left arm. “Bellamy’s pediatrician referred me to
“Bellamy’s pediatrician referred me to  After Bellamy woke up from surgery, the Pantojas were amazed to see their son move his left arm. He raised his arm up to his chest like he was showing off what he was not able to do before.
After Bellamy woke up from surgery, the Pantojas were amazed to see their son move his left arm. He raised his arm up to his chest like he was showing off what he was not able to do before.
 Plagiocephaly occurs when a baby develops a flattening on the back or side of the head. This occurs when a baby spends increased time in the same position. If left untreated, babies with plagiocephaly may develop asymmetries of the head, neck and face. Often, plagiocephaly can accompany torticollis, a condition that occurs when the muscles in a baby’s neck become stiff or tight, which causes the head to tilt to one side. It can affect a baby’s posture, causing them to favor one side of their body.
Plagiocephaly occurs when a baby develops a flattening on the back or side of the head. This occurs when a baby spends increased time in the same position. If left untreated, babies with plagiocephaly may develop asymmetries of the head, neck and face. Often, plagiocephaly can accompany torticollis, a condition that occurs when the muscles in a baby’s neck become stiff or tight, which causes the head to tilt to one side. It can affect a baby’s posture, causing them to favor one side of their body. Eli started wearing his helmet when he was 6 months old. When he first got the helmet, he wore it for an hour on and an hour off, and the number of hours were gradually increased each day over the course of five days. Eli was then able to wear the helmet for 23 hours a day. The Vasquezes took pictures of their son’s head every week. They say it was amazing to see the progression of his head from totally flat to almost perfectly round.
Eli started wearing his helmet when he was 6 months old. When he first got the helmet, he wore it for an hour on and an hour off, and the number of hours were gradually increased each day over the course of five days. Eli was then able to wear the helmet for 23 hours a day. The Vasquezes took pictures of their son’s head every week. They say it was amazing to see the progression of his head from totally flat to almost perfectly round.